Embarking on the path to understanding and managing ulcerative colitis requires a nuanced exploration of its diagnosis. This chronic inflammatory bowel disease, intricately entwined with the colon and rectum, presents a distinctive puzzle in the realm of gastrointestinal health. From the unique characteristics of this disease that set it apart to the diagnostic tools that provide clarity, it’s important to explore insights that transcend the clinical, empowering individuals on their quest for comprehension and effective management of ulcerative colitis.
What is Ulcerative Colitis?
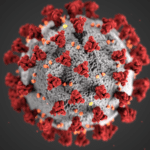
Ulcerative colitis is a chronic inflammatory bowel disease (IBD) characterized by inflammation of the colon and rectum. It is one of the two main types of IBD, the other being Crohn's disease. Unlike Crohn's disease, which can affect any part of the digestive tract, ulcerative colitis specifically targets the large intestine.
Some unique and key characteristics of ulcerative colitis make it easier to stay alert:
- Location of Inflammation: The inflammation in ulcerative colitis is typically continuous and begins in the rectum, gradually spreading to other parts of the colon. In severe cases, the inflammation can involve the entire colon.
- Nature of Inflammation: Ulcerative colitis causes inflammation of the innermost lining of the colon, leading to the formation of ulcers. The inflammation can result in various symptoms, ranging from mild to severe.
- Symptoms: Common symptoms include abdominal pain, persistent diarrhea, rectal bleeding, weight loss, and fatigue. The intensity and frequency of these symptoms can vary, and individuals may experience periods of remission and flare-ups.
How Is Ulcerative Colitis Diagnosed?
Reaching a conclusive diagnosis of ulcerative colitis involves a comprehensive approach, encompassing various assessments and diagnostic tools. Understanding the steps involved is crucial for individuals seeking answers about their digestive health.
Clinical Assessment
Clinical assessments and evaluations for ulcerative colitis include:
- Symptom Evaluation: The diagnostic journey often commences with a detailed discussion about the individual's symptoms. Persistent diarrhea, abdominal pain, rectal bleeding, unintended weight loss, and fatigue are key indicators that healthcare professionals carefully consider.
- Medical History: Beyond symptoms, a thorough exploration of the patient's medical history is vital. Family history, especially regarding inflammatory bowel diseases, can offer valuable insights into the likelihood of ulcerative colitis.
Laboratory Tests
Lab testing for ulcerative colitis includes:
- Blood Tests: Assessing inflammation markers, such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), aids in gauging the extent of inflammation in the body. Elevated levels may signify active disease.
- Stool Tests: Analyzing stool samples is another crucial step. This helps identify potential infections, assess inflammation, and detect the presence of blood, a common symptom in ulcerative colitis.
Imaging Studies
Imaging studies of ulcerative colitis include:
- Colonoscopy: Often considered the gold standard for diagnosis, a colonoscopy involves the insertion of a flexible tube with a camera into the rectum and colon. This allows direct visualization of the colon's lining, enabling healthcare professionals to identify inflammation, ulcers, and other abnormalities.
- CT Scan or MRI: In certain cases, imaging studies like computed tomography (CT) scan or magnetic resonance imaging (MRI) may be recommended. These provide a detailed view of the digestive tract and surrounding structures, helping evaluate the extent of inflammation.
Biopsy
Biopsy measures for ulcerative colitis include:
- Tissue Samples: During a colonoscopy, small tissue samples, or biopsies, are taken from inflamed areas. These samples are then examined under a microscope to confirm the diagnosis and determine the severity of inflammation. Biopsies are integral in distinguishing ulcerative colitis from other conditions.
Other Diagnostic Tools
Other diagnostic tools to diagnose ulcerative colitis include:
- Flexible Sigmoidoscopy: This procedure involves the use of a flexible tube to examine the lower part of the colon. While not as comprehensive as a full colonoscopy, it can provide valuable information.
- Upper Endoscopy: Although less common, an upper endoscopy may be performed to rule out involvement of the upper gastrointestinal tract.
Colonoscopy Guidelines for Ulcerative Colitis
Colonoscopies are integral to both diagnosing and managing ulcerative colitis. They involve routine biopsies to confirm diagnosis and assess inflammation severity, and they are crucial for surveillance, enabling early detection of complications like colorectal cancer and strictures. Initially performed to confirm ulcerative colitis presence, subsequent colonoscopies monitor disease progression and treatment effectiveness. Regular screenings are recommended for individuals with long-standing ulcerative colitis to mitigate colorectal cancer risk and evaluate stricture presence.
Aftercare Following Colonoscopy For Ulcerative Colitis
After the completion of a colonoscopy, individuals with ulcerative colitis should be mindful of specific post-procedure considerations:
Recovery Period
After a colonoscopy, individuals with Ulcerative Colitis may experience temporary bloating or gas. The body requires time to recover from the procedure. Resting is crucial during this period, and it's advisable to have someone accompany you home, ensuring a safe and comfortable return.
Dietary Considerations
Following a colonoscopy, healthcare providers often recommend a gentle diet, starting with easily digestible foods. This may include clear liquids and soft, bland options. Gradually reintroducing regular foods is a gradual process that allows the digestive system to ease back into its normal routine. Staying well-hydrated is paramount for a smooth recovery and to prevent dehydration.
Monitoring Symptoms
Post-colonoscopy, it's essential to closely monitor any changes in symptoms. While mild discomfort or minor bleeding may be expected, persistent or severe symptoms should be promptly reported to healthcare professionals. This vigilance ensures early detection of potential complications and timely intervention.
Medication Guidance
If medications were temporarily adjusted before the colonoscopy, it's crucial to resume the regular medication schedule as advised by the healthcare provider. Consistency in medication is vital for maintaining disease management and preventing flare-ups.
Beyond the diagnostic role of colonoscopies in managing Ulcerative Colitis, their significance extends to regular monitoring and surveillance. Equally important is the attention given to aftercare, ensuring a smooth recovery process and optimal symptom management specific to ulcerative colitis.
Decoding How To Get Diagnosed With Ulcerative Colitis With Northeast Digestive
Empower your well-being by consulting with our experienced gastroenterologists. If you're experiencing symptoms or have a family history of Ulcerative Colitis, schedule a consultation to explore personalized insights and, if necessary, undergo a vital colonoscopy. Your journey to digestive health starts with a proactive decision. Contact Northeast Digestive today and book your appointment with our expert team.